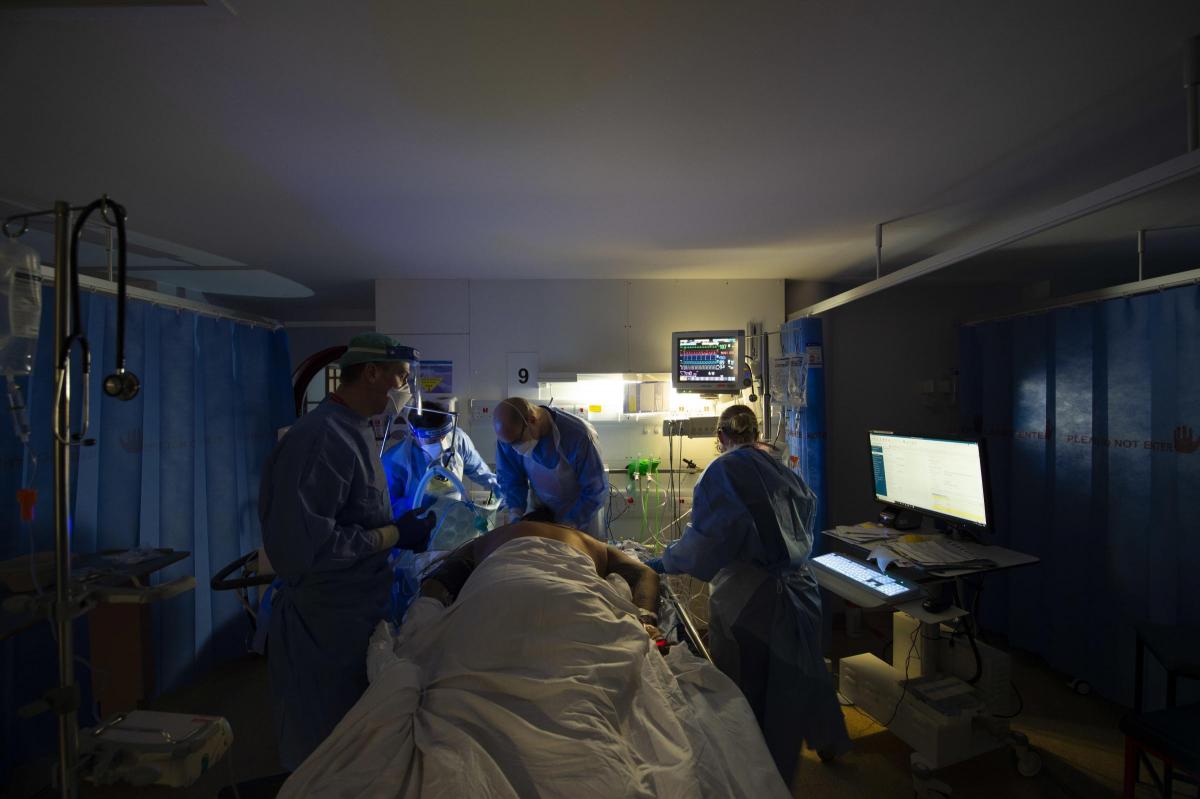
IT was a ghastly year. 'Absolutely horrendous' at times.
But it wasn't until January, just two months ago and some eleven months into the pandemic that 'the jaws of hell opened' at Bournemouth and Poole hospitals.
By the middle of that month, there 402 Covid positive (or blue) patients across the two sites and things were almost at breaking point. Almost.
Last Friday there were just nine blue patients with only two in intensive care -although it has taken longer get those ICU figures down.
That day chief executive of University Hospitals Dorset, Debbie Fleming, spoke frankly about the toll the last year has taken and the huge challenges ahead, in a wide-ranging interview on the eve of the lockdown anniversary.
One of the greatest of those challenges is the backlog of cases that has built up.
As of now it is a staggering 45,524 patients waiting, with 5,325 with a waiting time of more than 52 weeks.
These are known as long waiters.
But the Covid crisis is far from over Mrs Fleming warned as we cast an anxious glance across to what is happening in France, Germany and Italy.
She said: "No, it is definitely not over. We have a vaccine and the roll out has been tremendous so I do not believe we will see those kind of numbers again. It's such an achievement to have vaccinated 25 million plus people. By Sunday the figure was 26,853,407 first doses given.
"But he bit we have to focus on is ensuring that people do not take risks.
"We have to stay vigilant and continue with all the testing and make sure that as we unlock there are no surprises."
Around 17,000 vaccinations have been administered at the two hospitals, including their own staff, care home and other key workers."
Mrs Fleming reflected on the first wave in March last year when the hospitals had on average 80 patients on any given day.
"Even at that point we were all horrified and shut the hospital to visitors."
But this would be as nothing compared with what came later.
In the summer, on some days there were no Covid patients at all, leading to a real sense of optimism as the two hospital trusts merged formally in October, the culmination of an almost decade-long process.
"We always knew there could be second wave but I remember on that merger day feeling really, really positive and excited, that we had learned a lot, that we had got new drugs and better treatments.
"But soon afterwards, the jaws of hell opened from my point of view. It got worse and worse and worse and reached a crescendo in January.
"In October we had an outbreak at Poole Hospital, in November we had a series of outbreaks at Bournemouth Hospital. And this all as the infection rates in the community were going so much higher.
"So in the first wave we had eighty patients and that was flipping awful, but just compare that with the 402 patients by the middle of January.
"So many of our beds were filled with Covid patients and that was really challenging."
It was not until the autumn that the lateral flow testing regime for hospitals was ramped after the government finally made it a national priority.
The statistics make stark reading.
The cumulative cases, 3040. Cumulative deaths,740.
At the height of the crisis in January, staff sickness levels peaked at twice the normal rate.
Nearly 400 staff off symptomatic, 194 isolating and 75 shielding.
In total around nine per cent of all employees.
But there were still many others on duty some coming into work shocked and frightened each day, to do their job.
Some were traumatised. Others still suffering PTSD.
Mrs Fleming said the Bournemouth, Christchurch and Poole area has been one of the worst hit areas in the South West, in part because of the proximity to the South East.
Another issue was the large number of people who came down to visit family and friends over the short Christmas period.
The rate of infection in the BCP area was up to around 900 per 100,000 at one point, higher than the national average.
"As a trust we were particularly hit by the high infection rates locally," said Mrs Fleming.
One of the consequences for the chief executive on a personal level was less interaction with staff.
"I felt it was wrong for me to go wandering round the hospital as much as normal so I started doing videos which I found was an effective way to communicate.
"I wanted to thank staff for their work and shine a light on those who were less visible.
"There was a lot of national attention on intensive care units and emergency departments and I went to see them of course but the first people I visited were the porters and the kitchen, just some of the wonderful members of the team who don't the glory but who came in every day, frightened, really frightened, to do their job. I was really humbled by that.
"Everyone single member of staff has their own story, not just as someone who works in one of our hospitals, but also as a member of the community."
The time for a full national inquiry is soon but not now she insists.
"We aren't through this yet and haven't even lifted the lockdown but there does need to a full review. One thing we already know is we have all learned an awful lot."
Today everyone at the hospitals will be remembering staff and patients they have lost but they will also looking forward too.
And part of that looking forward is about getting back to some kind of normality and dealing with that backlog.
"I can remember being absolutely devastated when we only had a few people waiting more than a year. Normally I would expect to have none so the current situation is dreadful. We want to clear this."
These cases are not life-threatening but each one is a personal and difficult story.
The chief executive is proud that in a year of Covid and of merger, the scores from staff on how they feel about where they work and would they recommend it as a place to receive care have gone up.
"That is because of all our great people who have supported each other through all this."
Having reported on numerous occasions from both hospitals through the pandemic, the survey results are perhaps the least surprising thing I have heard in the past 12 months.










Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel